Premature ejaculation
| Premature ejaculation | |
|---|---|
| Classification and external resources | |
| ICD-10 | F52.4 |
| ICD-9 | 302.75 |
| MedlinePlus | 001524 |
| eMedicine | med/643 |
Premature ejaculation (PE) is a condition in which a man ejaculates earlier than he or his partner would like him to. Premature ejaculation is also known as rapid ejaculation, rapid climax, premature climax, or early ejaculation.
Masters and Johnson defines PE as the condition in which a man ejaculates before his sex partner achieves orgasm, in more than fifty percent of their sexual encounters. Other sex researchers have defined premature ejaculation as occurring if the man ejaculates within two minutes of penetration; however, a survey by Alfred Kinsey in the 1950s demonstrated that three quarters of men ejaculate within two minutes of penetration in over half of their sexual encounters.. Self reported surveys report up to 75% of men ejaculate within 10 minutes of penetration. Today, most sex therapists understand premature ejaculation as occurring when a lack of ejaculatory control interferes with sexual or emotional well-being in one or both partners.
Most men experience premature ejaculation at least once in their lives. PE affects 25%-40% of men in the United States. Because there is great variability in both how long it takes men to ejaculate and how long both partners want sex to last, researchers have begun to form a quantitative definition of premature ejaculation. Current evidence supports an average intravaginal ejaculation latency time of six and a half minutes in 18-30 year olds.[1][2] If the disorder is defined as an IELT percentile below 2.5, then premature ejaculation could be suggested by an IELT of less than about 2 minutes.[3] Nevertheless, it is well accepted that men with IELTs below 1.5 minutes could be "happy" with their performance and do not report a lack of control and therefore would not be defined as having PE. On the other hand, a man with 2 minutes IELT may have the perception of poor control over his ejaculation, distressed about his condition, has interpersonal difficulties and therefore be diagnosed with PE.
Contents |
Possible psychological and environmental factors
Psychological factors commonly contribute to premature ejaculation. While men sometimes underestimate the relationship between sexual performance and emotional well-being, premature ejaculation can be caused by temporary depression, stress over financial matters, unrealistic expectations about performance, a history of sexual repression, or an overall lack of confidence. Interpersonal dynamics strongly contribute to sexual function, and premature ejaculation can be caused by a lack of communication between partners, hurt feelings, or unresolved conflicts that interfere with the ability to achieve emotional intimacy. Neurological premature ejaculation can also lead to other forms of sexual dysfunction, or intensify the existing problem, by creating performance anxiety. In a less pathological context, premature ejaculation could also be caused simply by extreme arousal.
According to the theories developed by Wilhelm Reich, premature ejaculation may be a consequence of a stasis of sexual energy in the pelvic musculature, which prevents the diffusion of such energy to other parts of the body.[4]
One study of young married couples (Tullberg, 1999) reported that the husband's IELT seems to be affected by the phases of the wife's menstrual cycle, the IELT tending to be shortest during the fertile phase. Other studies suggest that young men with older female partners reach the ejaculatory threshold sooner, on average, than those whose partners are their own age or younger .
Possible physical factors
Science of mechanism of ejaculation
The physical process of ejaculation requires two sequential actions: emission and expulsion.
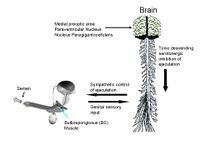
The emission phase is the first phase. It involves deposition of seminal fluid from the ampullary vas deferens, seminal vesicles, and prostate gland into the posterior urethra.[5] The second phase is the expulsion phase. It involves closure of bladder neck, followed by the rhythmic contractions of the urethra by pelvic-perineal and bulbospongiosus muscle, and intermittent relaxation of external urethral sphincters.[6]
It is believed that the neurotransmitter serotonin (5HT) plays a central role in modulating ejaculation. Several animal studies have demonstrated its inhibitory effect on ejaculation. Therefore, it is perceived that low level of serotonin in the synaptic cleft in these specific areas in the brain could cause premature ejaculation. This theory is further supported by the proven effectiveness of selective serotonin reuptake inhibitors (SSRIs), which increase serotonin level in the synapse, in treating PE.
Sympathetic motor neurons control the emission phase of ejaculation reflex, and expulsion phase is executed by somatic and autonomic motor neurons. These motor neurons are located in the thoracolumbar and lumbosacral spinal cord and are activated in a coordinated manner when sufficient sensory input to reach the ejaculatory threshold has entered the central nervous system.[7][8]
Several areas in the brain, and especially the nucleus paragigantocellularis, have been identified to be involved in ejaculatory control.[9] Scientists have long suspected a genetic link to certain forms of premature ejaculation. In one study, ninety-one percent of men who have had premature ejaculation for their entire lives also had a first-relative with lifelong premature ejaculation. Other researchers have noted that men who have premature ejaculation have a faster neurological response in the pelvic muscles. Simple exercises commonly suggested by sex therapists can significantly improve ejaculatory control for men with premature ejaculation caused by neurological factors. Often, these men may benefit from anti-anxiety medication or SSRIs, such as sertraline or paroxetine, as these slow down ejaculation times [1]. Some men prefer using anaesthetic creams; however, these creams may also deaden sensations in the man's partner, and are not generally recommended by sex therapists.
Premature Ejaculation Diagnostic Tool (Premature Ejaculation Test)
A diagnostic tool to help physicians and patients diagnose this condition has been developed. The methodology and results were published several times in medical congresses and peer reviewed medical journals.[10][11] The three different categories a patient can be classified to are: No PE; Probable PE; and PE.
Differential diagnosis
Premature ejaculation should be distinguished from erectile dysfunction related to the development of a general medical condition. Some individuals with erectile dysfunction may omit their usual strategies for delaying orgasm. Others require prolonged noncoital stimulation to develop a degree of erection sufficient for intromission. In such individuals, sexual arousal may be so high that ejaculation occurs immediately. Occasional problems with premature ejaculation that are not persistent or recurrent or are not accompanied by marked distress or interpersonal difficulty do not qualify for the diagnosis of premature ejaculation. The clinician should also take into account the individual's age, overall sexual experience, recent sexual activity, and the novelty of the partner. When problems with premature ejaculation are due exclusively to substance use (e.g., opioid withdrawal), a substance-induced sexual dysfunction can be diagnosed.
Other ejaculation disorder types
- Delayed ejaculation - Ejaculation takes a long time
- Retrograde ejaculation - Semen flows from the prostate gland into the bladder rather than exiting out of the penis.
- Inhibited orgasm in males[12]
Treatment
In mundane cases, treatments are focused on gradually training and improving mental habituation to sex and physical development of stimulation control. In clinical cases, various medications are being tested to help slow down the speed of the arousal response.
Masters and Johnson recommended a start and stop technique to increase the time until ejaculation. This requires a great deal of couple cooperation and communication, and may be difficult for some.
Another method is that of control instead of prevention. Performing routines such as Kegel exercises, which, as mentioned above, relate to gaining voluntary control of the PC muscle and thus give a person more control over ejaculation. When ejaculating, the control of this muscle is said to be lost, and thus, learning to maintain control of it can be of aid to some.
Management
To maximise the benefits of medications and behavioural techniques in the management of premature ejaculation it is important to have a comprehensive approach to the problem,[13]A thorough sexual history and assessment of general health and other sexual problems (if any) are very important. Assessing (performance) anxiety, guilt (associated with masturbation in many South-Asian men), stress and worry are integral to the optimal management of PE.3 When a sexual problem is managed inappropriately or sub-optimally, it is very likely that the condition will subside immediately but re-emerge after a while. When this cycle continues, it strongly reinforces failure that eventually make clients not to access any help and suffer it all their life. So, it is important to get a thorough assessment from professionals and therapists who are qualified to manage sexual problems. Internet-based information is good for gaining knowledge about sexual functioning and sexual problem but not for self-diagnosis and/or self-management.
References
- ↑ "Ejaculation delay: what's normal? [July 2005; 137-4"]. http://www.medicine.ox.ac.uk/bandolier/band137/b137-4.html. Retrieved 2007-10-21.
- ↑ Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, Boolell M (2005). "A multinational population survey of intravaginal ejaculation latency time". The journal of sexual medicine 2 (4): 492–7. doi:10.1111/j.1743-6109.2005.00070.x. PMID 16422843.
- ↑ Waldinger MD, Zwinderman AH, Olivier B, Schweitzer DH (2005). "Proposal for a definition of lifelong premature ejaculation based on epidemiological stopwatch data". The journal of sexual medicine 2 (4): 498–507. doi:10.1111/j.1743-6109.2005.00069.x. PMID 16422844.
- ↑ See for example Body of knowledge: an introduction to body/mind psychology by Robert L. Marrone, SUNY Press, 1990, ISBN 0791403874, 9780791403877, p. 104
- ↑ Böhlen D, Hugonnet CL, Mills RD, Weise ES, Schmid HP (2000). "Five meters of H(2)O: the pressure at the urinary bladder neck during human ejaculation". Prostate 44 (4): 339–41. doi:10.1002/1097-0045(20000901)44:4<339::AID-PROS12>3.0.CO;2-Z. PMID 10951500.
- ↑ Master VA, Turek PJ (2001). "Ejaculatory physiology and dysfunction". Urol. Clin. North Am. 28 (2): 363–75, x. doi:10.1016/S0094-0143(05)70145-2. PMID 11402588.
- ↑ deGroat WC, Booth AM (1980). "Physiology of male sexual function". Ann. Intern. Med. 92 (2 Pt 2): 329–31. PMID 7356224.
- ↑ Truitt WA, Coolen LM (2002). "Identification of a potential ejaculation generator in the spinal cord". Science 297 (5586): 1566–9. doi:10.1126/science.1073885. PMID 12202834.
- ↑ Coolen LM, Olivier B, Peters HJ, Veening JG (1997). "Demonstration of ejaculation-induced neural activity in the male rat brain using 5-HT1A agonist 8-OH-DPAT". Physiol. Behav. 62 (4): 881–91. doi:10.1016/S0031-9384(97)00258-8. PMID 9284512.
- ↑ Symonds T, Perelman MA, Althof S, Giuliano F, Martin M, May K, Abraham L, Crossland A, Morris M (2007). "Development and validation of a premature ejaculation diagnostic tool". Eur Urol. 52: (2): 565–73. doi:10.1016/j.eururo.2007.01.028. PMID 17275165.
- ↑ Althof S, Rosen R, Symonds T, Mundayat R, May K, Abraham L (2006). "Development and validation of a new questionnaire to assess sexual satisfaction, control, and distress associated with premature ejaculation.". J Sex Med 3 (3): 465–75. doi:10.1111/j.1743-6109.2006.00239.x. PMID 16681472.
- ↑ "Premature Ejaculation". Premature Ejaculation and Male Orgasmic Disorder. Armenian Medical Network. 2006. http://www.health.am/sex/premature-ejaculation/. Retrieved 2007-09-19.
- ↑ "Premature Ejaculation Help". http://www.sexualhealthindia.com/sexual-health/premature-ejaculation.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
External links